Table of Content
Nursing home coverage includes payment for room and board, as well as all necessary medical and non-medical goods and services. These can include skilled nursing care, physician’s visits, prescription medication, medication management, mental health counseling, social activities and assistance with the Activities of Daily Living . Nursing Home Medicaid is an entitlement, which means that all eligible applicants are guaranteed by law to receive the benefits. The Nursing Home program pays for long term care for persons who reside in skilled or intermediate care facilities. In order to qualify for this program, an applicant needs to meet certain financial and medical criteria. As we’ve discussed in previous blog posts, applicants must receive less that $2,163 in monthly income while having assets valued at no more than $2,000.

These documents will be needed for the official Medicaid application. One’s home is often their most valuable asset, and if counted toward the asset limit for Healthy Connections , it would likely cause them to be over the limit for eligibility. However, in some situations the home is not counted against the asset limit. If the applicant lives in their home and the home equity interest is less than $636,000 , then the home is exempt from the asset limit. Home equity interest is portion of the home’s equity value that the applicant owns, and the home’s equity value is the current value of the home minus any outstanding mortgage / debt against the home.
Medicaid Waiver Program for Assisted Living and In-Home Care
Fortunately, there are ways to meet these limits without jeopardizing one’s Medicaid eligibility. Prior to applying for long-term care Medicaid in South Carolina, it is imperative that seniors are certain all eligibility requirements are met. Persons who have income and / or resources in excess of the limit can benefit from Medicaid planning for the best chance of acceptance into a Medicaid program. To learn more about the long-term care Medicaid application process, click here.
For those who are eligible, Medicaid will pay for the complete cost of nursing home care, including room and board. Medicaid will pay for nursing home care on an ongoing, long term basis for however long that level of care is required, even if it is required for the remainder of one’s life. In many cases it is not necessary to transfer to another nursing home when payment source changes to Medicaid NF. Many nursing homes are also certified as a Medicare skilled nursing facility , and most accept long-term care insurance and private payment.
New Requirement For Medicaid Effective November 2017
If a senior resides in a nursing home, the Medicaid beneficiary must reside in a Medicaid-certified nursing facility for their care to be covered. States may specify the types and limitations of some services that can be provided, but federal regulations require that certified nursing homes must offer specific services at a minimum and at no charge to Medicaid residents. NF services for are required to be provided by state Medicaid programs for individuals age 21 or older who need them. States may not limit access to the service, or make it subject to waiting lists, as they may for home and community based services. Therefore, in some cases NF services may be more immediately available than other long-term care options. NF residents and their families should investigate other long-term care options in order to transition back to the community as quickly as possible.
However, all states provide the service, and in practice there is no distinction between the services. Like most HCBS Waivers, the South Carolina Community Choices Waiver is not an entitlement program. Instead, there are a limited number of enrollment spots , and once those spots are full, other eligible applicants will be placed on a waiting list before receiving benefits. The Medicaid resource limit for a single person in New York State for 2021 is $15,900.
Nursing Facility Services Links
Citizen residing in South Carolina in order to qualify for South Carolina’s Medicaid Program. You will also often be asked to provide a significant number of financial records for the five years leading up to the application. Typically, this means an Applicant will have to provide bank statements, tax returns, account statements from other financial institutions, and any relevant deeds, just to name a few. Lastly, all applicants applying for nursing-home coverage must be over the age of 65.

After an applicant has been approved for nursing home coverage through Healthy Connections , they need to choose which Medicaid-approved nursing home they will live in. Even though Medicaid nursing home coverage is an entitlement, Healthy Connections will only cover stays and care in approved nursing homes. This South Carolina Department on Aging webpage has a locator tool to help individuals find Medicaid-approved nursing homes in their area.
Medicaid NF services are available only when other payment options are unavailable and the individual is eligible for the Medicaid program. Rather, the Medicaid SNF benefit, like its Medicare counterpart, seems to have been viewed as a cost-effective alternative for recipients who would otherwise spend protracted stays in more expensive acute care settings. To be eligible for Healthy Connections , a person has to meet certain financial and functional requirements. Any Healthy Connections beneficiary who receives nursing home coverage must give most of their income to the state to help pay for the cost of the nursing home. They are only allowed to keep a “personal needs allowance” of $30 / month. This can be spent on personal items such as clothes, snacks, books, haircuts, cell phones, etc.

These programs have varying financial and medical eligibility requirements, as well as benefits. Further complicating eligibility are the facts that the requirements vary with marital status and that South Carolina offers multiple pathways towards Medicaid eligibility. Be blind.Most states automatically provide Medicaid eligibility to applicants who apply and are deemed eligible for Supplemental Security Income . However, there are a handful of states who use the same eligibility guidelines but require an applicant to file separate SSI and Medicaid applications to receive both benefits.
For information on what your state provides, see our series of articles on state-by-state eligibility for Medicaid long-term care. If you have limited assets and a low income and you need help paying for nursing home or assisted living care, Medicaid might help you pay for your care. Medicaid is a joint federal and state program, and the states have some flexibility in setting the benefits they will offer and the eligibility criteria for those benefits.
Enrollment in this program is voluntary, and members may change their plan monthly. The average cost of Nursing home care in South Carolina is $6,596, so penalties can become very costly for a family that has not planned appropriately for Medicaid. The application requires an extensive amount of supporting documentation. Families should be prepared to spend many hours gathering financial documents. This website provides a free, fast and non-binding Medicaid eligibility test for seniors.
For a single applicant in 2022, the asset limit for HCBS Waivers in South Carolina is $2,000, which means they must have $2,000 or less in countable assets. In all 50 states and the District of Columbia, Medicaid will pay for nursing home care for persons who require that level of care and meet the program’s financial eligibility requirements. Readers should be aware that the financial requirements and the level of care requirements vary based on the state. Furthering the complexity is that the financial requirements change based on the marital status of the Medicaid beneficiary / applicant.
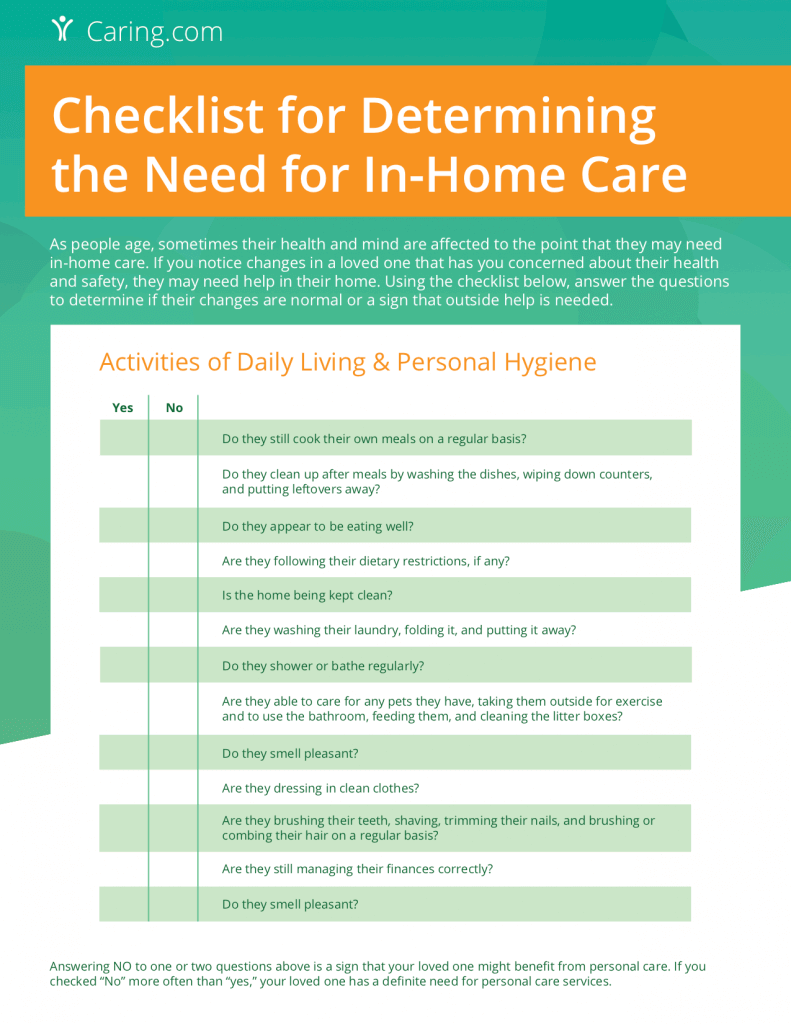
For long-term care services via the Regular Medicaid program, a functional need with the activities of daily living is required, but a NFLOC is not necessarily required. Like all states, South Carolina Medicaid pays for nursing home care for state residents who are medically and financially eligible for such care. SC Medicaid also offers Medicaid programs for seniors who require nursing home level care or have slightly lesser care requirements and do not wish to reside in a nursing home. South Carolina Medicaid, which is called Healthy Connections, will cover the cost of long-term care in a nursing home for eligible South Carolina residents who require a Nursing Facility Level of Care.
In addition to providing care in nursing homes and assisted living facilities, SC Medicaid pays for non-medical services and supports to help frail seniors remain living in their homes. South Carolina residents have to meet an asset limit and an income limit in order to be financially eligible for Aged Blind and Disabled Medicaid / Regular Medicaid through Healthy Connections . For a single applicant in 2022, the asset limit is $8,400, which means they must have $8,400 or less in countable assets. Almost all income is counted (IRA payments, pension payments, Social Security benefits, property income, alimony, wages, salary, stock dividends, etc.) other than COVID-19 stimulus checks and Holocaust restitution payments. All 50 states have financial and level of care eligibility criteria for Medicaid-funded nursing home care. The financial eligibility criteria consist of income limits and countable assets limits.
The cost of care, room, meals, and medical supplies are all included in the daily rate. Medicaid pays a fixed daily rate so a nursing home Medicaid beneficiary does not have to pay any part of the cost. All assets of a married couple are considered jointly owned regardless of the long-term care Medicaid program for which one is applying.
No comments:
Post a Comment